This article was written collaboratively by the Advanced Industries Practice. The authors include Stephanie Balgeman, Ben Meigs, Stephan Mohr, Arvid Niemöller, and Paolo Spranzi.
Although much remains unknown about COVID-19, scientists have established that the coronavirus is highly contagious and transmitted via air. Studies suggest that it primarily spreads when infected people cough, sneeze, or talk—actions that expel respiratory droplets containing particles of coronavirus in combination with mucus or saliva. If these droplets land on or are inhaled by others nearby, they could transmit the coronavirus.1 Touching doorknobs, computer screens, or other surfaces on which droplets have landed may also lead to infection. The now-common guidelines for wearing masks and physical distancing—typically, by remaining six feet away from others—reflect these observations.
Questions remain, however, about whether tiny coronavirus particles, of about 0.1 microns in size, can become airborne and travel greater distances. Although heavy droplets, of about five to ten microns, usually travel less than one meter before settling, smaller droplets may evaporate, leaving virus particles, referred to as aerosols, suspended in the air.2 A recent study demonstrated that coronavirus particles may be active for up to three hours after their release.3 Although the World Health Organization (WHO) initially held that the coronavirus could not be spread through aerosols, it recently reversed its stance. The WHO guidelines now state that airborne transmission of the coronavirus may be possible indoors, especially for people who spend extended periods in crowded, poorly ventilated rooms.4 The WHO’s turnaround came after the organization received an open letter from 293 scientists asking the organization to reconsider its position on airborne transmission.5
Given the concern about airborne transmission, building managers, safety experts, and others might take steps to optimize ventilation and airflow indoors and limit viral spread. Some simple moves may help (see sidebar “Low-tech strategies for preventing airborne viral transmission”). But this may also be a good time to think about improving air quality in buildings by significantly changing heating, ventilation, and air-conditioning (HVAC) systems or by making physical changes to manage indoor airflows.
Control-setting changes and upgrades to HVAC systems
HVAC systems6 can potentially spread a virus across rooms when high-speed air flows past an infected person to others, something that has been shown with Severe Acute Respiratory Syndrome in 2004.7 If airborne transmission is also possible with the coronavirus, a few control-setting changes and upgrades may help decrease the risk of spread through this route. If building managers take such actions, they might help their tenants feel more comfortable amid all the uncertainty about the coronavirus (see the sidebar “Earning the trust of tenants”).
One step that technicians could take involves configuring ducted HVAC systems to increase the rate of exchange with fresh fresh air from outside the building to reduce recirculation. Adjusting the settings may also help. Instead of shutting down overnight or on weekends, for instance, the HVAC system could run without interruption to increase the replacement of air and minimize airflow speeds.
In buildings with old or inflexible systems, technicians might consider upgrading HVAC hardware. Some of the most important might include these:
- replacing fixed-speed fan motors with variable-speed ones to enhance the control of airflow and allow for a minimum setting that produces lower speed airflow
- introducing sophisticated airflow-control systems, such as those that are sensitive to pressure, to allow for smoother adjustment of airflows
- installing high-performance air-purification systems, as discussed in the next section
Options for air purification
Numerous technologies can purify air. Filtration is the most common and typically the most effective method for HVAC systems (Exhibit 1). Other technologies, including irradiation and thermal sterilization, inactivate biological particles in the air without removing them. HVAC systems can also incorporate ionic purifiers, ozone generators, and other devices for cleaning air.

Filters in residential or commercial HVAC systems are usually installed either at an air inlet or outlet or within the central air-handling unit. Since external air that flows into an HVAC system may be contaminated, especially in metropolitan areas where buildings are in close proximity, technicians sometimes install a pre-filter for incoming air.
The mechanical filters in HVAC systems have tangled fibers that trap particles too large to fit through the openings. Mechanical filters have different ratings, based on the percentage of particles they remove, with the highest rated typically used in surgical or clean-room applications. Exhibit 2 shows selected filters and their ratings from organizations based in the United States. Ratings standards in other countries may vary.

High-Efficiency Particulate Air (HEPA) filters are most effective at removing small particles. To meet this qualification under the US ratings system, filters must remove 99.97 percent of particles of 0.3 microns. Minimum Efficiency Reporting Value (MERV) filters are assigned ratings according to their ability to filter out large particles (from 0.3 to 10.0 microns in size). MERV filters with ratings of 17 or higher are comparable to HEPA filters and may be referred to by that term.8 Like the air-conditioning systems in most homes, commercial buildings generally have filters rated MERV 12 or lower. Only some air conditioners can accommodate HEPA filters, and technicians must configure them properly and replace them regularly.
Upgrading HVAC systems by incorporating higher-grade filters can be very expensive and is not always feasible. What’s more, even a HEPA filter will not eliminate all concerns about airborne transmission. Although a NASA study documented that HEPA filters can stop particles as small as 0.1 microns—the approximate size of the coronavirus—other direct research is limited, and the official US ratings system specifies their efficacy only for particles of 0.3 microns.9 More research is needed to definitively determine a minimum filtration rating that will eliminate infectious coronavirus particles from air.
Airflow management
While studies are still ongoing about how the coronavirus spreads via air, evidence suggests that measures to change indoor airflow patterns could play a role in reducing transmission. Three main principles apply:
- encouraging a vertical laminar rather than turbulent airflow
- ensuring a slow, steady air speed
- directing potentially contaminated air out of rooms and away from people
In-room airflows
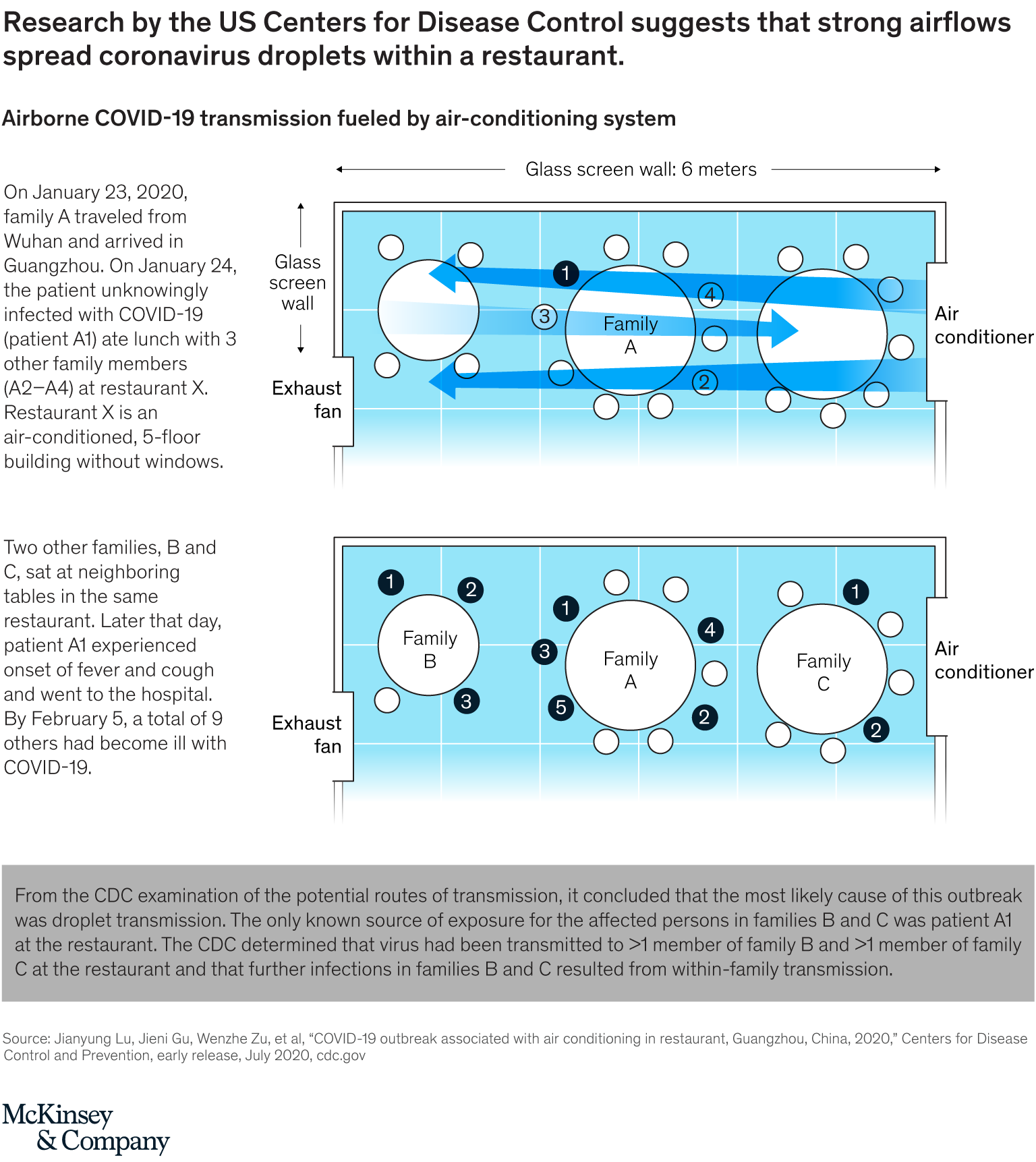
The World Health Organization recently acknowledged that some evidence about in-room transmission is worrisome. In addition, after analyzing a transmission event at a restaurant in China, the US Centers for Disease Control and Prevention (CDC) concluded that an asymptomatic patient transmitted the virus to families at two nearby tables (Exhibit 3).10 Based on the restaurant layout, seating arrangements, and smear samples from air-conditioning inlets and outlets, the CDC found that the coronavirus was likely transmitted when strong airflows from a nearby air conditioner spread large droplets from the infected person. These droplets traveled more than one meter—further than usual, but less than the distance aerosols can typically travel.
Changing airflow patterns to create laminar vertical airflow—air moving in the same speed and in a straight path—may effectively prevent the airborne transmission of coronavirus particles.11 This principle is already used to prevent the spread of particles in several settings. For instance, clean rooms and hospital operating rooms minimize contamination via sophisticated systems to direct air from the ceiling to the floor with laminar flow. On commercial aircraft, ventilation systems are configured to blow air vertically from ceiling to floor to reduce the spread of contaminated air within the cabin.
Would you like to learn more about our Advanced Electronics Practice?
Creating airflows that are close to laminar will involve far more than changing HVAC settings. In new construction, for instance, builders must include a sufficient number of air outlets. In existing structures, technicians may need to upgrade the outlets in HVAC systems—for instance, by adding some outlets in the space provided by suspended ceilings. In some cases, technicians may replace outlet covers, which are normally designed to mix and distribute air, with covers that produce laminar flows. For both new and existing buildings, the placement of air outlets is critical and must be based on planned occupancy, room architecture, furniture placement, and other factors that influence airflows.
In some cases, building managers might want to add physical barriers, such as partitions that separate open space, to manage airflows within rooms. They could also install in-room sterilizers to reduce viral concentrations, but these increase turbulence and are thus recommended primarily for offices occupied by only one person.
Inter-room airflow
Some building managers and others may want to take steps to prevent contamination between rooms—something that could occur if the coronavirus is found to spread via airborne transmission. Technicians should identify how air moves through rooms before installing new devices or upgrading HVAC systems. Their evaluations could include a blower-door test, which involves creating calibrated pressure in a room and then monitoring the flow and leakage.
Several options, some involving HVAC upgrades and others focusing on simpler changes, could address any problems detected. These solutions might include installing doors or air curtains, generating overpressure above suspended ceilings, and sealing any gaps in them (Exhibit 4).

Individual protection
In some workplaces, close physical contact is difficult to avoid, which makes viral transmission risk higher. To date, however, no commercial products protect airflows within individual workstations, such as a specific position next to an assembly line or an employee’s desk. Innovators may introduce some solutions for individual protection, such as those that involve adapting principles from airflow-control units or ventilation hoods, especially if the evidence for airborne transmission of the coronavirus continues to climb.
As economies worldwide reopen, healthcare officials have good reason to fear a second wave of COVID-19. Offices have traditionally accommodated large numbers of people and were designed to foster interaction and collaboration. Manufacturing shop floors sometimes require employees to work in close proximity. Schools, with their historically strained budgets, will find it especially hard to separate students from one another and from faculty. Hospitals have put off many elective procedures and noncritical surgeries for months and could begin seeing more patients in closer proximity.
Governments, trade groups, HVAC manufacturers, building engineers, and regulators may want to consider optimizing airflows whenever possible. Changes to ventilation systems, air-purification systems, and airflow management will probably be the focus of their work in this area.
Disclaimer: The document summarizes a preliminary view on best practices, potential design concepts, and approaches to ventilation and airflows that could limit virus spread in buildings. At this time, more research is needed on the airborne transmission of COVID-19 and the best measures for preventing viral spread. References to specific products or organizations are solely for illustration and do not constitute any endorsement or recommendation.

